Health Equity and Patient Care
One of the most critical issues for the Community Oncology Alliance (COA) and the COA Patient Advocacy Network (CPAN) is health equity. While some issues, like PBMs, can be addressed through legislative and regulatory action, health equity is a broader issue that requires sweeping changes to the access and affordability of cancer care.
Host Rose Gerber, MS, COA’s director of patient advocacy and education, is joined by nationally known Richard L. Martin III, MD, MPH, Tennessee Oncology’s director of health equity and community engagement, to discuss the realities of addressing health equity inside a community oncology clinic, including overcoming language barriers, providing financial assistance for underinsured and economically disadvantaged patients, and understanding cultural norms around cancer treatment.
When a patient is seeking a diagnosis or being treated for cancer, their health is not the only factor to consider. Where a patient lives, their ethnicity, economic status, and even their religious background can significantly affect how, when, and where they can receive treatment. By collaborating with patients to accommodate and address these factors, we can make cancer care more equitable. This not only improves treatment outcomes but also enhances patients’ quality of life, underscoring the crucial role that plays in their care.
Health Equity Objectives
Why Equity? Why Now?
In making the argument for health equity, there is a confluence of aligned incentives and an impetus for change. These are based on values like justice, solidarity, integrity, and compassion, as well as the duties of the Hippocratic oath and service to all. The Hippocratic oath, which health care providers take, and the principle of service to all, underscore the ethical basis for the argument for health equity. This alignment underscores providers’ duty and commitment to practicing professionalism and ensuring informed, shared decision-making, which in turn will improve performance by raising standards, increasing safety, and improving the patient experience. Together, these will improve outcomes. Better systems are inherently more equitable.
As new treatments are created, there is an obligation to ensure that everyone has access to them. Failure to do so increases the disparity in health equity, and the “have-nots” can fall farther and farther behind the “haves.”
Improvement comes not just in cancer medicines but also in supportive care. Palliative care reduces avoidable spending and utilization in all settings:
- Inpatient – fewer readmissions with a lower daily cost
- Outpatient – fewer hospital and emergency department admissions
- Skilled Nursing – fewer hospital and emergency department transfers
- Home-Based – lower costs for at-home care, reduced food insecurities
The value of reduced cost and improved quality of life translates to increased survival rates.
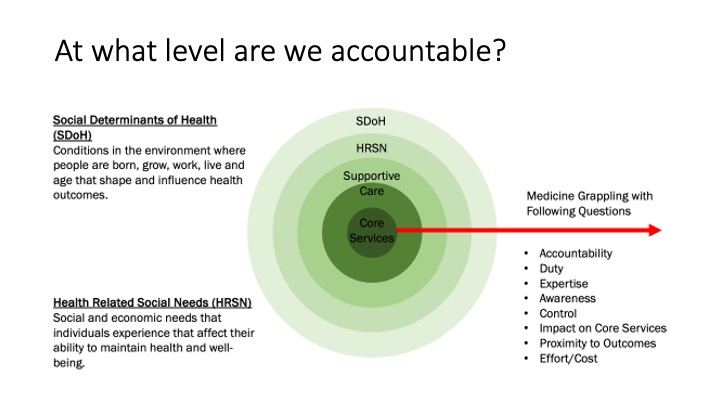
There are multiple levels of cancer care accountability:
- Social Determinants of Health (SDOH) are conditions in the environment. Where people are born, grow, work, live, and their age shape and influence health outcomes.
- Health Related Social Needs (HRSN) are those social and economic needs that individuals experience that affect their ability to maintain their health and well-being.
Providers grapple with the SDOH and HRSN as these factors affect the ability to provide core services and how well they can serve patients with cancer.
Getting Buy-In
The question remains about the best way to get buy-in. The best option may be a two-pronged approach. Buy-in may need to come from the top down by involving a combination of executive, corporate, and payer stakeholders and from the bottom up by involving staff, patients, and community stakeholders. Several changes reflecting this strategy are being implemented. The Food and Drug Administration (FDA) has begun requiring a diversity plan for clinical trials to increase the number of participants from under-represented groups in drug testing.
A more rigorous Enhanced Oncology Model (EOM) has been introduced to improve the quality of care and equitable health outcomes for all EOM beneficiaries, including but not limited to:
- Incentivizing care for under-served communities
- Collecting beneficiary-level sociodemographic data
- Identifying and addressing HRSN
- Improving shared decision-making and care planning
- Providing continuous quality improvement (QCI)
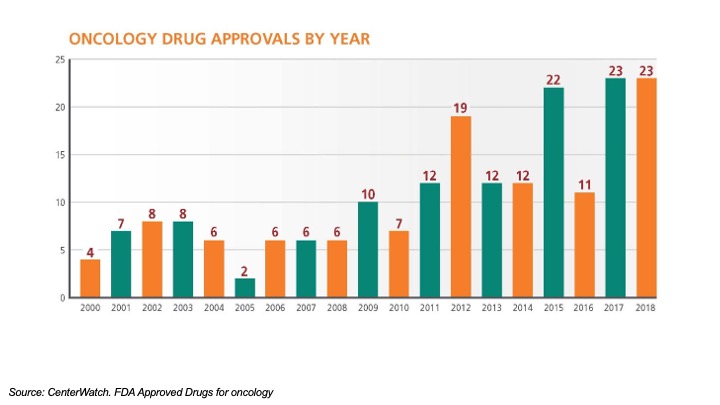
The explosive growth in new cancer therapies requires that providers know which therapies work for which groups of patients with cancer. They can fall behind if they do not know who might benefit from any given treatment, which is information the broader clinical trials could provide. Additionally, payers are reluctant to pay for therapies that cannot be demonstrated to benefit the patient.
There is often a 17-year lag from basic research to develop a new drug to clinical trials and approval and then to use in clinical practices across the health care system. Sometimes, there can be immunotherapies patients would like to consider. Because African American patients were under-represented in the long completed clinical trials, assessing if a patient would benefit from this treatment option can be challenging. Given the cost, payers may balk at the cost of such therapies for which a treatment benefit cannot be predicted.
One way to address this issue is to use Trial Matching Services, which provide patient-facing clinical trial matching. Services input such patient data as:
- Age, diagnosis, location
- Common somatic mutations
- Prior lines of therapies, comorbidities, performance status
- Distance patient is willing to travel, preferred form of therapy
As the specificity of the patient data increases, the number of appropriate trials decreases, determining the specific clinical trials for which the patient is likely to be eligible and interested.
What is Health Equity?
Health equity is removing disparities in care. That does not mean taking from some by giving to others. It means giving the proper care to the right people at the right time. This includes all the various stakeholders involved:
- Pharmaceutical companies
- Health data companies
- Clinical practices
- Diagnostic companies
- Insurance companies
- Patients
- Community organizations
Equity starts with understanding people and what they need. Greater community engagement makes the community informed, involved, and directed as an advisor, collaborator, and leader.
The Institute of Medicine says that equity is one of the hallmarks of high-quality medical care. Equity needs to be layered throughout everything a practice does.
This is internal in the form of the workforce and external in the community involvement. For example, there is no point in enrolling patients in clinical trials to provide drugs they cannot afford.
From Plan to Action
The move from plan to action requires building internal and external capacity. The Tennessee IMPACT Program is comprised of:
- Advanced practice providers’ opportunities for leadership
- Shelf stable food program across four practice service regions
- Three domains
- Service
- Education
- Advocacy
The strategy is to:
- Align outreach efforts with Tennessee Oncology’s core mission
- Build capacity by growing volunteers and a training pipeline
- Improve sustainability by replicating successful projects
Getting the Right Drug to the Right Patient at the Right Time
When providers are determining the best cancer treatment protocols, they review the current data, including:
- Cell of origin
- Stage
- Molecular
- Prior lines of therapy
- Concurrent therapies
- Performance status
- Comorbidities
- Consent
The future of health care, which will maximize the best overall cancer treatment plan for the greatest number of people, is patient-centered and evidence-based and requires not just looking at the cancer facts but also at the human factors. Consequently, many now envision a future when molecular profiling will yield such specific and granular data that it will herald a new era of “personalized” cancer therapy at the individual level.
How to Be an Impactful Clinical Equity Champion
Patient scenarios are the best place to start discussing health equity because they impact what a clinician does about the real world.
Patient Scenario
- 43YO, African American male
- Newly diagnosed metastatic colon cancer
- No significant prior medical history
- Works out
- Cares about fitness
- Family history of cancer: mother died in her 60s due to colon cancer
The patient is devastated and wonders how this could have happened to him. What do you tell him?
We have known for 25-30 years that among African American individuals, colon cancer presents at an earlier age, despite there not being any racially focused screening differences. The difference in the incidence of cancer based on race and ethnicity is something we should embrace as it would help to formulate screening and treatment protocols. This will aid in providing the best care at the best time. Sometimes, a difference based on race is a proxy for differences in access and affordability.
Scenario Action
In 2021 the updated Colorectal Cancer (CRC) screening recommendations were changed:
- Screening recommendations were extended to an earlier age cohort
- Average risk age was lowered from 50 to 45-49
- No racially focused recommendations were issued
The rationale for expanding screening guidelines was that while the incidence of CRC has always been high among young African Americans, the incidence is now increasing in young whites and Hispanics/Latinos. There is insufficient empirical evidence on the benefit or harm of earlier CRC screening in African Americans. As a result, the National Cancer Institute Cancer Intervention and Surveillance Modeling Network’s (NCI CISNET’s) modeling does not support different screening strategies based on race.
Take Aways
- Better systems are more equitable
- Equity is foundational across cancer care services
- Make it easy by repurposing current operations for HRSN and SDOH
- Venturing out always begins with a first step
- Stay humble and listen; you are not the expert!
- Build human capacity which is aligned with supporting diverse people
- Commit and hold yourself accountable
- Keep showing up!
Summary
Advocacy Chats are regular virtual 30-minute educational conversations about cancer advocacy and policy. Each month features a new topic and special guests joining us. Patients, survivors, caregivers, and other cancer care advocates are all invited to join us for these no-charge and interactive virtual events. Summaries of previous Advocacy Chats are available on the CPAN website.
CPAN Advocacy Chats are regular virtual 30-minute educational conversations about cancer advocacy and policy with a guest speaker invited to discuss issues important to patients and advocates. Summaries of previous Advocacy Chats are available on the CPAN website.
Past Advocacy Chats