The Latest Cancer Policy Updates from Washington
The Latest Cancer Policy Updates from Washington
In anticipation of the upcoming Community Oncology Alliance (COA) Hill Day, this Community Oncology Alliance Patient Advocacy Network (CPAN) chat with COA’s Director of Patient Advocacy and Education, Rose Gerber, MS, and Managing Director, Nicolas Ferreyros, explored the changing landscape of Washington and how 2024 has been full of movement on key issues affecting the deliverability, accessibility, and cost of cancer care. As the year proceeds, advocates will need to know what bills and policies are being promoted or changed by lawmakers and regulators.
Rose and Nick covered the major cancer policy developments from the first half of the year, what bills and projects are being considered on Capitol Hill, and COA’s plans for the rest of 2024, including the May Hill Day. They also recapped policy sessions at the 2024 Community Oncology Conference and what speakers there thought about various policy items making their way through Congress. Transcripts from the Conference sessions are available to all registered attendees on the COA YouTube channel and the COA website.
The Political Reality: Washington Is a Mess
The political reality is Washington has been a mess for a while. It remains a mess, and there is no sign that things will change before the election in November 2024. Many congressional districts are gerrymandered, so the advantage to one party or the other remains entrenched and does not change, no matter who is elected. Legislators often will not collaborate with members of the other party making compromise and bipartisanship increasingly rare.
Democrats barely control the Senate, and Republicans barely control the House of Representatives. This means both parties must work with the other to get something passed. Rather than doing that, what has happened is that little legislation is getting passed and:
- Government shutdowns have been threatened
- Several short-term funding bills were passed in lieu of a full budget
- After six months, Congress finally passed a budget
- Election season often means an ”us versus them” mentality
- Legislators take time away from Washington to fundraise and campaign
- 33 Senate seats and all 435 House seats are up for election
- Many provider champions are retiring
- Representatives Bucshon, Burgess, Eshoo, and Wenstrup
- Senators Braun and Romney
- Many question if anything will get done before the election
While legislators are elected, much of the work is done by senior staffers. Things have become so difficult that half of the senior staff are so fed up that they may quit.
Voter Concerns: Health Care “Costs” and Affordability
Over half of all voters say inflation, the cost of everyday expenses, and housing and health care are why they describe the economy negatively. Seventy-four percent of all adults say they are worried about being able to afford unexpected medical bills.
Politicians love to focus on health care and drug costs, particularly in an election year. Drug prices and health care costs are perennial big issues in Washington. Every elected official in the U.S. has promised to address prices and vowed to reduce the cost of drugs. “Big Pharma” is a frequent punching bag for politicians – particularly with the passage of the Inflation Reduction Act (IRA), which will allow for Medicare drug price negotiations. The IRA passage has allowed politicians to claim that as big win and turn their focus to pharmacy benefit managers (PBMs), hospitals, and insurers.
These are the very issues on which COA and CPAN are focusing in 2024.
COA’s 2024 Policy and Advocacy Priorities
Every year, the COA leadership team brings together representatives of practice leadership, practice administrators, the Government Affairs and Policy (GAP) Committee, the pharmacy network, and the advocacy network. Collectively, the group determines what remains undone, what policy issues are top of mind, and what keeps practices awake with worry. This evolves into the list of issues COA will focus on for the next year.
The 2024 list of issues includes:
- Ensuring sustainable payments and reimbursement
- Pharmacy benefit manager (PBM) reform
- Addressing anti-competitive hospital policies and regulation
- Provider wellness and workforce issues
- Prior authorization and utilization management reform to protect patients
- Finding permanent solutions to cancer drug shortages
- Supporting system transformation and new payment models
- Improving cancer health equity
This list, in turn, becomes the policy and legislative issues most watched by COA.
Active Washington Policy and Legislative Issues on COA’s Radar
PBM Abuses and Reform
The Abuses
The single biggest focus for practices and their patients is PBMs. This is an issue with multiple components all simultaneously under watch and review:
- Centers for Medicare and Medicaid Services (CMS) prohibiting practices from delivering cancer drugs to patients
- “Non-profit” hospitals and 340B program
- Community oncology provider payment/reimbursement
- IRA drug negotiation technical fix
- Cancer drug shortages
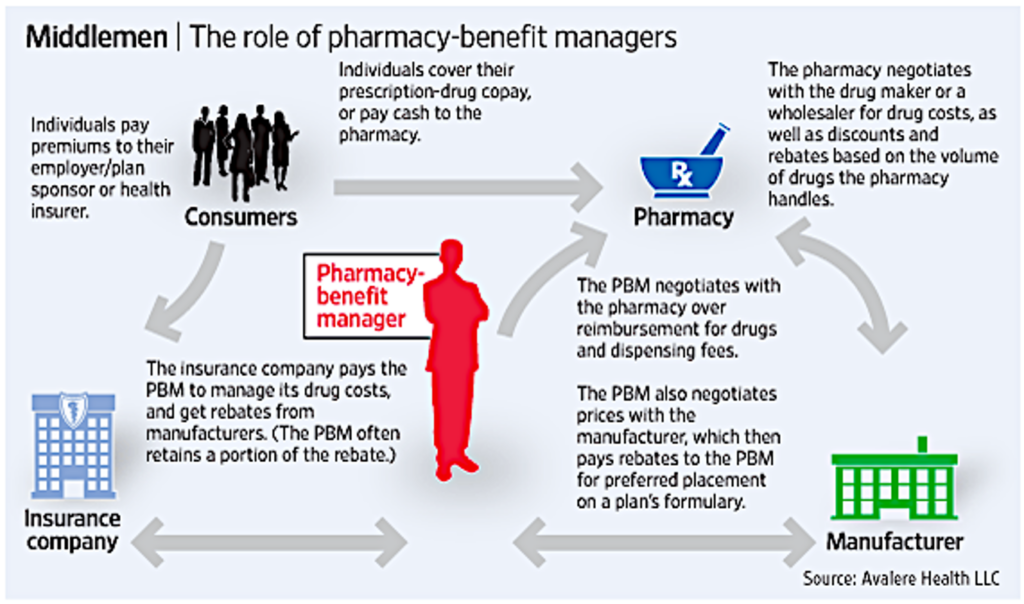
PBMs are large, often for-profit corporations hired as middlemen to manage prescription drug benefits on behalf of health insurers, Medicare Part D drug plans, large employers, and other payers. Most people do not know about PBMs because they are middlemen who are not always visible to patients. PBMs silently control what, when, and where patients can access prescription drugs.
PBMs have an impact on patients by:
- Delaying and denying patients with cancer from getting their drugs
- Forcing the use of mail-order pharmacy
- Using “fail-first” step therapy, prior authorization, and other utilization management to ensure the most profitable (to the PBM) drugs are used
- The most profitable drug is not always the most effective drug or the drug that is the least expensive for the patient
PBMs have an impact on practices by:
- Forcing underwater reimbursement
- Excluding pharmacies from PBM networks
- Moving drugs that are a medical benefit to become a pharmacy benefit
COA has published eight volumes of PBM patient horror stories detailing specific, actual cases where patient care was delayed, denied, or worse.
The Reform
Many wonder if there will ever be meaningful PBM reform. Pre-COVID and pre-IRA, PBMs were happily functioning in the shadows. The Democrats barely acknowledged PBMs and focused on “big pharma” while the Republicans acknowledged PBM issues though they were not a major focus.
Post-COVID and the IRA, PBMs were in the spotlight. At least 25 PBM-focused bills were being pushed through various investigations and committees. The Federal Trade Commission (FTC) was working on a major PBM report. The Government Accounting Office (GAO) was producing a report on PBM rebates. Bipartisan action on PBMs was underway.
Multiple hearings were putting PBMs in the hot seat and there was a promise of even more hearings in the future. Seven congressional committees were working on various combined PBM bills. The House of Representatives’ work included the Energy and Commerce, Ways and Means, and Education and the Workforce Committees. In the Senate, the Finance, Health Education, Labor and Pensions, and Commerce Committees were also working.
The stage was set for PBM reform from Congress in 2024, but the bills failed to make it into budget packages. Without a legislative package, there was no vehicle for reforms to proceed. COA hopes the momentum will not stop.
One of the most important messages that COA will deliver at the upcoming Hill Day is keeping the much-needed reform momentum going. Realistically, not much is likely to happen before the election as legislator focus turns to campaigning. However, after the election, there is a lame-duck period where legislators who lost their election are still in office, and the newly elected legislators have not yet taken office. In this period, there is often an opportunity for compromise and accomplishment with less political consequence. This year, there is an opportunity for things to happen in the lame-duck period because, previously, things were so close to actual reform.
There were several commonalities of the legislative action earlier in 2024 that could result in PBM reforms, such as:
- Transparency – reporting requirements on drug prices, rebates, formulary, benefit design
- Banning Spread Pricing – occurs when PBMs reimburse pharmacies less than what they make from drug plans and keep the “spread” as profit
- Rebate Passthrough – requiring PBMs to pass on 100 percent of rebates, fees, and discounts to plan sponsors
- Reduce Patient Out-of-Pocket Costs – tie cost sharing to the negotiated net price instead of the list price
- Delinking Drug Prices from PBM Profits – prohibiting PBMs from earning a profit based on drug list price by implementing a flat dollar compensation for their services
CMS Reinterpretation of Drug Delivery: A Stark Law Violation?
The pharmacies within most community oncology practices dispense the infused and oral drugs used to treat patients with cancer. This allows for close pharmacist engagement through the entire patient journey, from pretreatment through treatment monitoring, and therefore a multidisciplinary team approach. That process has been interrupted.
- During COVID, practices were allowed to deliver oral drugs to their patients.
- CMS halted delivery with end of the COVID Public Health Emergency (PHE).
- CMS now says practices are not allowed to deliver oral drugs to patients.
- Drugs must be picked up in person.
- Friends, family, or caregivers are also not allowed to pick up oral drugs.
- CMS now considers oral drug delivery a Stark Law violation against self-dealing.
- CMS says beneficiaries can get drugs through mail order from Part D plan sponsors (aka PBMs).
- PBM mail order has shown to be an endless source of problems and delays.
- This rule change is a nightmare for patients and practices.
- PBMs have begun trolling for patients.
- Oncologists’ prescriptions are being abandoned in favor of PBM substitutions.
- COA has an ongoing lawsuit against CMS to resolve this issue.
- COA is working with Congress on a legislative fix.
- Seniors’ Access to Critical Medications Act (H.R. 5526 & S. 3458)
What an Advocate Can Do: Engage, Educate, Advocate
One of the most important things advocates can do is to spend time advocating with their members of Congress. The constant turnover in staff often means that despite previous meetings, the current staff members may be unaware of the COA and CPAN issues. Ongoing education is necessary.
Advocates can have influence at the state level, as well. By meeting with state officials and various state regulatory agencies, such as insurance commissioners, pharmacy boards, and others, it is possible to enact state laws to address the most important COA and CPAN issues.
Capturing and telling advocates’ patient stories brings complex issues into an individual patient-centric focus. COA needs the stories of real patients to illustrate the impact of legislation and highlight the need for reform. This is a way every advocate can make a difference.
Summary
Advocacy Chats are regular virtual 30-minute educational conversations about cancer advocacy and policy. Each month features a new topic and special guests joining us. Patients, survivors, caregivers, and other cancer care advocates are all invited to join us for these free and interactive virtual events. Summaries of previous Advocacy Chats are available on the CPAN website.
CPAN Advocacy Chats are regular virtual 30-minute educational conversations about cancer advocacy and policy with a guest speaker invited to discuss issues important to patients and advocates. Summaries of previous Advocacy Chats are available on the CPAN website.
Past Advocacy Chats