How Cancer Rehabilitation Benefits Patients
One of the often-overlooked consequences of cancer is how debilitating the disease and treatment can be and what accommodations may be necessary to continue life as usual as possible. Cancer rehabilitation addresses all those issues and offers the support most patients need. When the Advocacy Chats first started in 2020, the focus was mostly on policy issues affecting patients and cancer care. Rose Gerber, MS, COA’s director of patient advocacy and education, reminded all that periodically the Chats will introduce new topics and resources from areas that have an immediate impact on patient care. This topic falls into that category.
Alaina Newell, PT, DPT, is the director of education for ReVital Cancer Rehabilitation. In addition to being double board certified as a Clinical Specialist in Oncologic Physical Therapy and a Clinical Specialist in Women’s Health Physical Therapy, she is also a Lymphology Association of North America (LANA) Certified Lymphedema Specialist.
She explained how cancer rehabilitation is a valuable resource for patients with cancer. Those patients and caregivers who have been through cancer treatment – chemotherapy, radiation, pharmaceutical therapy, and multiple surgeries – know how that impacts a patient’s emotional and physical health. While treatment has many issues affecting patient health, long-term survivors know that there are also many ongoing post-treatment issues.
Why Do We Need Cancer Rehabilitation?
On New Year’s Day in 2016, a patient, Arlene, went into the hospital with abdominal pain and swelling. She left the hospital four days later following a de-bulking surgery with a diagnosis of Stage IV ovarian cancer. Six weeks prior to her surgery she had run a Half
Ironman Marathon, and now she decided to step away from her high-stress job to find a deeper connection with her son and to spend more days outdoors, with fewer nights in hotel rooms and business meetings. Over the next five years and two months, she did just that. Along with her oncology team, her cancer physical and occupational therapists made sure she accomplished her goa
Arlene needed cancer rehab to allow her to get back to the mountains she wanted to climb, swim, bike, run, and travel with her son; to attend her son’s girlfriend’s college graduation, but most importantly to have the time, energy, and strength to find peace at the end of her life. Cancer rehab restored her posture and strength following surgery and helped rebuild her strength, energy, and endurance so she could tolerate over 50 chemotherapy infusions over five years while hiking mountains and running relay races.
Not all cancer survivors have the desire to run a Half Ironman Marathon or set similar goals, but all cancer survivors have goals and desires they hope to achieve during their cancer journey. Perhaps a patient with head and neck cancer wants to be able to drive safely because they can turn their head, or a woman with breast cancer wants to be able to hug her child without experiencing pain. For a man with lung cancer to be able to climb the stairs to his bedroom may be a critical thing in his life. These are all reasons why cancer rehab is needed.
How Many Patients Need Cancer Rehab?
Studies show that 60-90 percent of individuals impacted by cancer have at least one need and could benefit from specialized rehabilitation services. That translates to 10.2 million survivors out of the 17 million cancer survivors in the United States who need specialized cancer rehabilitation.
These needs are diverse among survivors and include such things as:
- Pain
- Cancer-related fatigue
- Weakness and deconditioning
- Difficulty with recreation and participation
- Numbness/pain in hands and/or feet
- Trouble walking or balance challenges
- Falls or near falls
- Cognitive decline “chemo brain”
- Difficulty with daily activities
- Arthralgia and myalgia (joint and muscle pain)
- Soft tissue changes or scarring
- Speech and swallowing challenges
- Lymphedema
- Pelvic health issues (bladder, bowel, sexual)
All of these needs impact patients’ ability to participate fully in life by attending kids’ soccer games or church, going to the farmer’s market, or doing daily activities, such as getting dressed, personal hygiene, or making dinner. While some of these conditions, such as “chemo brain” or fatigue, are both common and obvious, others are less common and more subtle.
It takes time for providers to determine patients’ needs and other areas where cancer rehab may be beneficial. Often times patients will respond when asked a direct question, but full discovery may rely on what family members notice and mention. Patients may not be willing to admit changes, but family members often observe a patient’s struggle with tasks that previously were easier. Initially, therapists will screen and question to identify needs and areas where therapeutic treatment may help. They frequently apply objective performance measures to better understand how patients function and areas where they may need help. Patients may also be screened for cognitive health and mental and emotional changes. While cancer rehabilitation does not directly address mental health, therapists can make referrals to other professionals when there is a need.
How Many Patients Who Need Cancer Rehab Actually Get It?
Of the 10 million survivors who need cancer rehabilitation, less than two percent have their rehabilitation needs are addressed. Typically, the conditions that are addressed are the ones that are obvious, such as a patient who falls and now has a broken hip or a patient who has an infection that has resulted in swelling and edema.
The life impact of needing an extra hour every morning to get dressed or sleeping in a chair in the living room because the climb to the bedroom is too much or asking a spouse to put on compression hose every morning and take them off every night can be huge. Patients have reported that they can no longer walk their dogs when the real problem is they do not trust themselves enough to bend over to clean up after their pets. The inability to overcome these lesser-known cancer side effects can be a powerful detractor from daily living.
While small, these are the things that make life more color
Where Cancer Rehab Is on the Cancer Continuum
Cancer rehabilitation has a role throughout the entire cancer experience. Therapists can work with patients as they go through pre-diagnosis and diagnosis to address the issue of preventative care and the steps patients can take to achieve and maintain a better state of health. Cancer rehab can anticipate what is coming and optimize patient support. During the treatment phase, cancer rehab continues to address issues of prevention, as well as restoration and support to help patients continue life as undisturbed by cancer and cancer treatment as possible. This phase addresses rehab from three vantage points – to restore function, to support to prevent further decline or to make accommodations, and, then again, to work to restore once treatment is completed. This continues into the follow-up period after treatment by helping to reduce the symptom burden. If a patient reaches a point where palliative or end-of-life care is needed, cancer rehab continues to support the patient.
Regardless of which stage a patient may be in, the patient remains at the center of rehabilitation efforts to prevent, support, and maintain as normal a life as possible. This includes retaining as many aspects of their former life as possible. It is important to remember that the cancer continuum is not linear. There are ups and downs; ground may be lost. There can be setbacks. Cancer can actually be more like a bouncing ball.
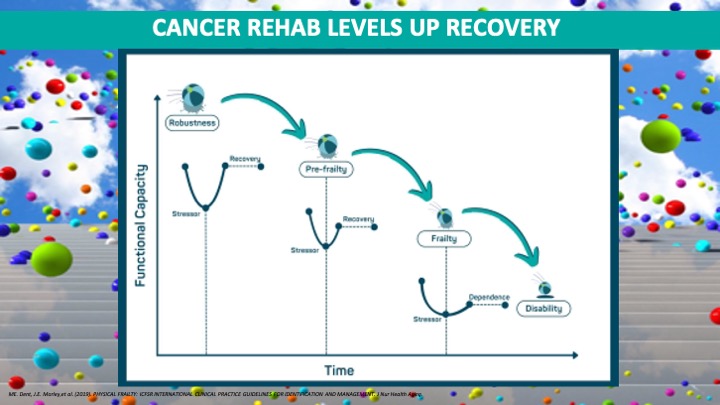
Cancer rehabilitation is a big part of getting patients to bounce back as much as possible by bringing their functional capacity to the highest level possible while acknowledging that in some cases patients will not bounce all the way back. In those cases, rehab works to make the accommodation and allow patients to retain as much of their previous life as possible.
Rehab Improves Cancer Outcomes
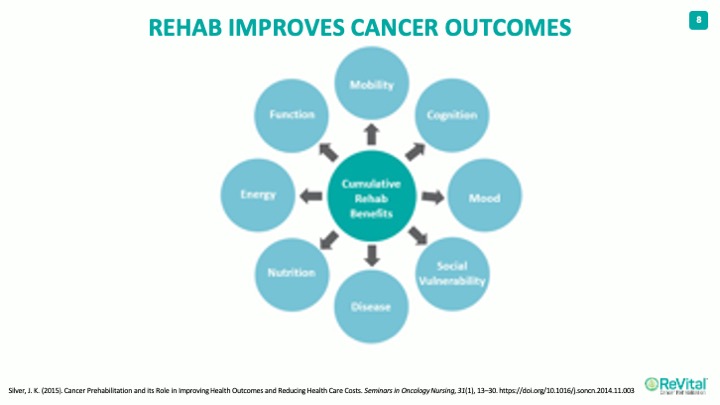
Rehab affects every aspect of a patient’s life. The cumulative benefits of cancer rehab work to improve:
- Cognition
- Mood
- Social ability to integrate into the community
- Disease
- Nutrition
- Energy levels
- General functioning
- Mobility
This reduces the symptom burden on the patient and improves the ability to tolerate more cancer treatments. Cancer rehab focuses on treating all aspects of a patient’s life, so they are truly living and not just alive.
Though cancer rehabilitation may be unfamiliar to many, studies have confirmed its contributions to patient care. A study published in Rehabilitation Oncology looked at patient-reported outcomes as well as performance-based measures of function and revealed that patients report cancer rehab improved the following:
- Global physical health
- Participation in social roles and activities
- Grip strength
- Decrease in fall risk
How Cancer Rehab Fits into the Cancer Care Standards and Guidelines
In 2013, the Institute of Medicine report, “Delivering High-Quality Cancer Care” stated that cancer rehab should be part of the cancer care team. The National Comprehensive Network promotes cancer rehabilitation services across three areas: survivorship, cancer-related fatigue, and adult cancer pain. In 2020, the Commission on Cancer directly named cancer rehab services and part of the standard of care emphasized the focus on quality care. There was a recommendation that the services be offered either on-site or by referral and defined the types of services that should be included.
An applicable quote from Dr. Atul Gawande in “The Checklist Manifesto: How to Get Things Right” stipulates:
“The volume and complexity of what we know has exceeded our individual ability to deliver its benefits correctly, safely, or reliably.”
By working in partnership with the entire cancer care team, cancer rehab clinicians provide the support patients need.
How Cancer Rehab Clinicians fit into the Cancer Care Team
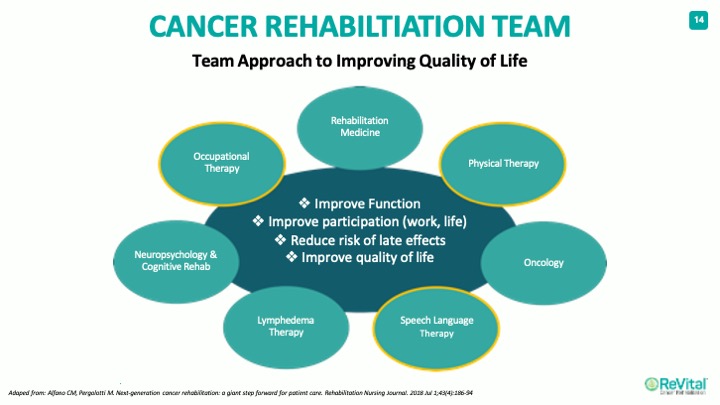
There are many on the cancer rehab team often focusing on occupational, physical, and speech therapy usually in both acute care and outpatient settings. Some patients will need only one type of therapy while others will require multiple specialists.
What Makes Cancer Rehab Unique?
Cancer rehab differs from traditional rehab because of the specialized knowledge of the medical management of cancer. This includes taking into consideration:
- Safety precautions and restrictions
- Effects of cancer on daily life
- Rehab considerations
The holistic care approach to cancer rehab incorporates several factors, such as:
- Screening for and addressing all cancer and treatment-related side effects
- Multi-disciplinary team (physical, occupational, speech, and language therapy)
- Treatment throughout the cancer continuum
Cancer Rehabilitation in Action
If we go back to the introductory patient, Arlene, her cancer rehab made things happen and allowed her to meet her goals. She was able to make several trips with her son. She attended her son’s girlfriend’s graduation. Rehab even enabled her to run a Half Ironman Marathon just a few months before her passing. At the end of the day, cancer rehab made it possible for her to achieve her big life goals over five years despite her cancer. She credits her whole cancer team with the support that made so many things possible and enabled her to consult different members of her team for help with different pieces of her life.
About ReVital Cancer Rehab
ReVital Cancer Rehab sees patients both in the clinic and via tele-rehab. Just like other forms of therapy, cancer rehab is covered by insurance. Available in 21 states its mission is to deliver outcomes that matter to patients throughout their cancer journey by understanding their needs and goals and providing specialized, comprehensive services at the hands of compassionate, dedicated clinicians. The therapists work to establish comprehensive cancer rehabilitation as a standard of care for people affected by cancer.
CPAN Advocacy Chats are regular virtual 30-minute educational conversations about cancer advocacy and policy with a guest speaker invited to discuss issues important to patients and advocates. Summaries of previous Advocacy Chats are available on the CPAN website.
Past Advocacy Chats